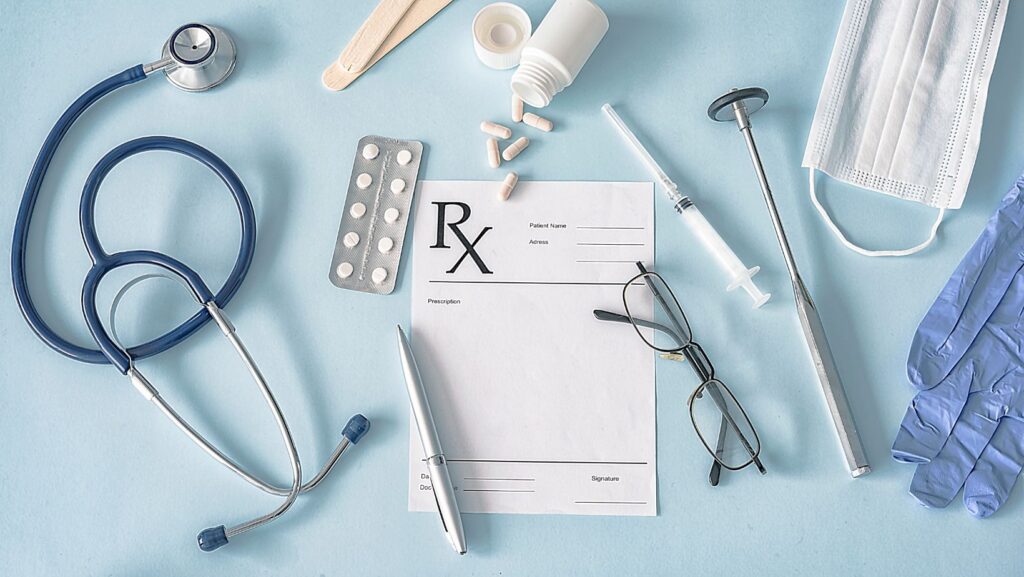
Which of the Following is Not Included in Comprehensive Major Medical Plans
Navigating the world of health insurance can be a daunting task. One common misconception is that comprehensive major medical plans cover every possible health issue. Unfortunately, that’s not the case. There are several services and treatments that these plans typically don’t cover.
In this article, I’ll shed some light on those gray areas. We’ll delve into what’s not included in comprehensive major medical plans. From alternative therapies to certain prescription drugs, you might be surprised to learn what’s left out.
By understanding these exclusions, you can make more informed decisions about your healthcare. Whether you’re considering a new plan or reassessing your current one, it’s vital to know what’s covered and what’s not. So, let’s dive in and unravel the often confusing world of health insurance.
Why are Certain Treatments/Services Not Included?
Understanding why certain services and treatments are not included in your comprehensive major medical plan can equip you with the knowledge to navigate the healthcare landscape more effectively. It’s important to remember that these exclusions are not arbitrary, they often have solid reasoning underpinning their absence from plans.
Experimental or Investigational Treatments
Often, comprehensive major medical plans do not cover experimental or investigational treatments. The primary reason is due to the uncertainty around these treatments’ effectiveness and safety. Insurance companies will typically only cover treatments that are proven to be safe and effective – they often follow the medical community’s consensus on what is considered “standard of care”. Experimental or investigational treatments due to their very nature, can be uncertain in their outcome and therefore pose a financial risk that insurers prefer not to take.
Cosmetic Procedures
Cosmetic procedures are typically procedures that are performed not for health reasons but to improve one’s physical appearance. These include operations like nose jobs, facelifts or liposuction. As these procedures are usually elective and not medically necessary, they are often excluded from comprehensive major medical plans. However, there might be exceptions if the procedure is reconstructive and required due to an accident or disease.
Alternative and Complementary Medicine
Alternative and complementary medicine treatments like acupuncture, chiropractic or homeopathy are commonly excluded from comprehensive major medical plans. While there is growing scientific evidence supporting these treatments, they are still viewed as outside the mainstream medical practices by many healthcare professionals and insurance companies. Also, because the effectiveness of these treatments may vary greatly from person to person, they often don’t fit neatly into the insurance models for cost prediction and risk assessment.
Differences in coverage can be confusing and lighting the way can be invaluable in navigating your healthcare decisions. However, it’s vital to acknowledge that insurance companies have healthcare advisers and medical directors who assess treatments and services’ efficacy before deciding whether to include them in their plans or not.
Common Treatments/Services Not Covered by Comprehensive Major Medical Plans
Let’s tackle this one by one.
Dental Care
Often, Dental Care isn’t part of comprehensive major medical plans. While a lot of people perceive dental care as essential healthcare, it’s typically considered a separate category. Mostly, you’ll find this covered under dental insurance and not necessarily a medical insurance plan. Just bear in mind, though – always check your policy details to be certain about coverage specifics.
Vision Care
Similarly, Vision Care – including eye exams, glasses, or contact lenses – is another service not typically included. Again, these sorts of health aspects are usually under specific vision coverage plans. However, major medical plans could include treatments for eye injuries or diseases.
Hearing Aids
Interestingly enough, even something crucial as Hearing Aids is often not part of comprehensive medical plans. The price of hearing aids can be exorbitant, but unfortunately, most insurance providers see them as elective procedures. Just like the above, it’s a good practice to confirm this with your insurer.
Long-Term Care
Despite being a significant aspect of healthcare for older people, Long-Term Care services are often not included. This includes things like custodial care, nursing homes and assisted living. These sorts of services demand a different kind of insurance, usually referred to as long-term care insurance.
Infertility Treatments
Finally, even though they’re incredibly important for those struggling to conceive naturally, Infertility Treatments are also commonly excluded. The rationale being, these treatments are considered elective and medically optional. But hold on, there might be medical plans out there with coverage for some sort of fertility treatment, so never miss to look into the specifics of your policy.